Learning to live with lockdown - our expert guide to coping with an enforced stay-at-home lifestyle
-
Research
- Health and Wellbeing
Posted on 19 May 2020
The loss of familiar structures and routines during the Covid crisis is taking its toll on our mental health. In this blog, our experts offer some advice on how to avoid feeling low during lockdown.

Throughout the early months of 2020, people around the world experienced a sudden major change to our lifestyles, which is a possible threat to our mood and longer-term mental health.
Lockdown and physical distancing measures linked to COVID-19 meant that many of the activities we used to do to keep us on an even keel were no longer possible. There is concern that these changes to our usual activities will be related to marked increases in mental health difficulties in the population.
Depression is more common in people with long-term physical health conditions than in the general population. One explanation of this is that the health condition stops the person from undertaking activities that in the past kept them feeling well. If someone is no longer able to go shopping, meet up with friends, and so on, they may start to feel low. They are no longer in touch with things in their world that had a naturally ‘anti-depressant’ effect for them.
There are clear parallels between the restrictions faced by people with long-term health problems and those faced by us all at present, particularly given the uncertainty about when and how the constraints will be eased.
The Mental Health and Addiction Research Group at the University of York and Hull York Medical School has over the last decade led research looking at Behavioural Activation for people with long-term conditions. This blog talks about some of the research we’ve been involved in, but also points out how the approach may be useful for all of us at the moment.
Behavioural Activation model of depression
How can we understand the potential consequences of the COVID-19 restrictions on our lifestyles for our mental health? And what can help? Behavioural Activation (BA), a treatment for low mood, may offer some insights. In particular, the idea of ‘functional equivalence’, a strategy commonly used when working with people with long-term health conditions, may be useful when thinking about our own mood during covid-related restrictions.
Behavioural Activation is based on operant conditioning principles. This is an old psychological theory, but it’s one that has stood the test of time. In brief, it states that if we want to understand behaviour, predict behaviour, and – perhaps most importantly – help people to change it, we need to look at when and where behaviours occur (the context) and how those behaviours work for us in that context (their function). If a behaviour works for us in some way in a specific context, we’ll learn to do more of it. If not, we’ll do less of it.
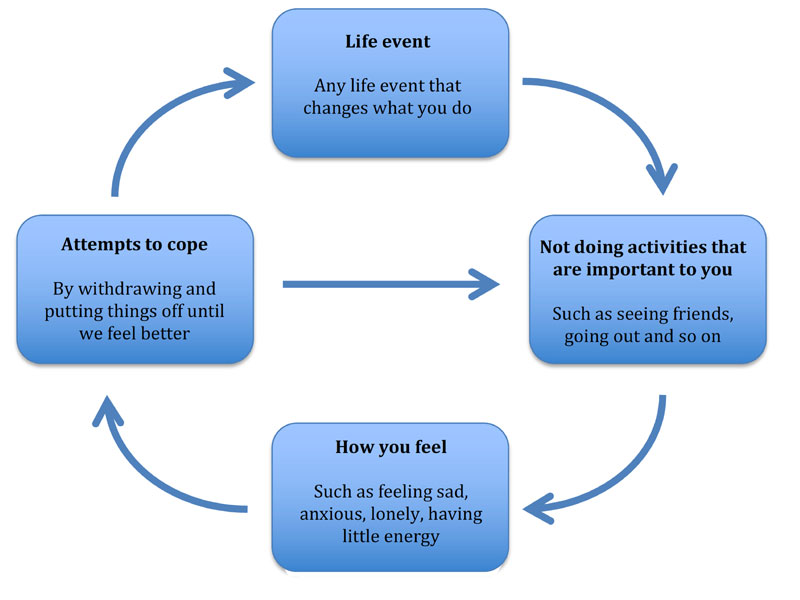
Psychologists have used operant conditioning principles to help us to understand depression. A simple version of this approach is summarised in the figure below, a model that we’ve used with participants in randomised trials of Behavioural Activation that we’ve conducted over the last decade. The basic idea is that if our life changes very suddenly our behaviours can struggle to keep up; sometimes we can’t adapt quickly enough to the new situation. As a result, we can get cut off from those things in life that are meaningful or important to us, and this can lead us to feel low. Understandably, in response, we try to cope. One way of coping that we use, particularly when feeling low, is to avoid things or to put things off until we feel better. This may work in the short-term for us, but in the long-term it means we end up doing even fewer of those activities that are important or meaningful to us. As the figure shows, this can set up a cycle that keeps low mood going.
Figure: Behavioural Activation cycle of low mood
Treatment principles
Psychologists have also used this approach to develop treatments for people with depression. One advantage of the treatment is that it is simple: it boils down to just four strategies. When training people to deliver Behavioural Activation, we talk about an R2D2 treatment:
- Reintroduce previous behaviours
- Replace ‘old’ behaviours with ‘new’ ones
- Decrease avoidance and withdrawal behaviours
- Develop ways of triggering helpful behaviours.
It’s the replacing ‘old’ behaviours with ‘new’ – or more formally looking to introduce ‘functionally equivalent’ behaviours – that we’ve found particularly helpful when working with people with long-term conditions who are experiencing low mood. We think this principle may be useful for us all while covid-related restrictions are in place, because we face the same challenges: we can no longer do those activities that we used to do to keep ourselves feeling well.
Using functionally equivalent behaviours to help improve mood
A first step is to think about what important activities are restricted and what they did for us in the past. When working with people experiencing depression, we choose an important activity that the person can no longer do and ask questions such as these:
- How did that activity help you?
- How did that behaviour work for you?
- What did the behaviour get you out of life?
Here’s a typical (fictionalised) example that we use in our treatment for people with long-term conditions. Susan has Chronic Obstructive Pulmonary Disorder, heart problems, and arthritis. Before she developed these long-term conditions, she liked to go out to a café in town two or three times a week. If we talked to Susan about this, she might identify these functions:
- ‘I really liked the toasted sandwiches’
- ‘I didn’t have to cook’
- ‘I got some fresh air’
- ‘I liked to talk to the owner – she made me laugh’
- ‘I liked how I could support a local business’
- ‘It stopped me and my husband living in each other’s pockets 24 hours a day’
- ‘On the way there, I would sometimes go to the Post Office to pay some bills’
- ‘It gave a bit of structure to my week’.
What can we learn from doing this with Susan?
One behaviour can have many functions. What is striking is how even one fairly simple behaviour can have many functions. Without thinking about it too much, Susan could identify eight ways going to the café helped her keep well. If we spent longer on this, we could probably identify other ways it helped.
Pleasurable, routine and necessary behaviours. Another point is that there is more to a behaviour that keeps us feeling happy than just pleasure. There are examples in Susan’s list of routine and necessary activities as well as pleasurable ones. A general rule in Behavioural Activation is that you need a balance of these activities to feel well.
Reducing is as important as increasing. The functions of a behaviour can include reducing things (for example, not cooking, not living in each other’s pockets) as well as increasing things as a way to maintain your mood. Susan and her husband may well love each other, but they don’t want to spend all day together, everyday.
Once we have identified all the functions of a behaviour, the next step is to think about alternative or new behaviours that may serve the same function as the previous one. From working with people to help them do this, we’ve found that the first ideas people have are often behavioural ‘close cousins’. If we can no longer go running we tend naturally to think of similar physical activities that look a bit like running. This may work sometimes, but Behavioural Activation encourages us to think more broadly and creatively. It is not the form of a behaviour (what it looks like) that matters but what it does for us or gets us out of life (its function). A new activity may look radically different to the original one, but still serve the same function. The other point we’ve found is that it is unlikely there will be a single behaviour that will serve all the same functions as an important ‘old’ behaviour. It may take several new activities to replace all of the functions of one ‘old’ behaviour.
With Susan, we’d work with her to think through each of the eight functions and identify new activities she could try that are still possible (‘functionally equivalent’ behaviours). Whether we were doing this before covid restrictions or during them may make a difference to what activities Susan could try, but the principle would be the same. What did the activity get Susan out of life? What new activities could she try to get the same things? For example, with Susan we’d discuss what other ways there are of socialising – and specifically ‘having a laugh’ with others. We’d also look at how Susan could structure her day and her week so her and her husband spend the amount of time together that works for both of them. We’d do this for each of the functions she’d identified. Often we’ll suggest using a diary to help plan the next week around these new activities.
While this approach is often used in Behavioural Activation when people have long-term health conditions, for any of us during covid restrictions, it may be worth thinking in terms of ‘functional equivalence’ as a way of looking after our mood. The idea would be to follow the same steps:
- Identify a behaviour that is important to you or helps you stay well, but at the moment you are no longer able to do because of covid restrictions
- Think about all of the different functions of that behaviour (including pleasurable, routine and necessary ones, and thinking about how it decreased as well as increased things)
- For each function, try to identify alternative behaviours that may get you the same thing out of life and that you can currently do – even if they look radically different
- Try these new behaviours out
- Repeat for other important or meaningful behaviours.
It may also help to consider these additional pointers that we use in Behavioural Activation:
- Experiment with behaviours: if you can think of two or three possible behaviours for one of the functions, try them all out; do the same for the other functions you’ve identified
- Experiment long enough to see what works: it may take a few weeks to see a benefit (there is often an ‘internal lag’; it may take a few weeks for thoughts and feelings to catch up with changes to activities)
- Work from the ‘outside in’: rather than wait to feel better (the inside) before trying the new behaviour (the outside), start with the behaviour (the outside) as a route to feeling better (the inside).
Does it work?
There are now many randomised trials of Behavioural Activation for depression. The conclusion from these is that it’s effective in helping reduce depressive symptoms. Interestingly, there is also evidence that it works as well as other well-established psychological treatments, such as Cognitive Behaviour Therapy (CBT). Our research group, for example, was involved in a large trial (over 400 people), the COBRA study, which directly compared CBT and Behavioural Activation in people with major depression. Both were effective, but there were no differences at all between the effectiveness of the two treatments.
We’ve also looked at Behavioural Activation as a preventative treatment for older adults, most of whom had a long-term physical health condition. This trial, the CASPER study, looked at over 700 older adults who had some low mood, but did not yet meet criteria for major depression. We found that the treatment reduced by about half the number of older adults who went on to become depressed a year later.
We were just about to start a new trial of Behavioural Activation for older adults with multiple long-term conditions, the MODS study, when covid restrictions took hold. We have worked rapidly to alter that trial to make it suitable for COVID-19 restrictions and people who are shielding. We’ll start offering Behavioural Activation treatment for this in the next few weeks, with the treatment delivered by phone.
Seeking help
While it is worth trying this approach out by yourself, there is good evidence that once someone’s low mood gets more severe or serious, it’s likely that they’ll need additional help from others. The good news is that there is also very solid evidence that getting this type of additional help does work, so if you are struggling, do make use of the various forms of formal support that are on offer.
The starting point for receiving formal help is typically your GP. In addition, students at the University of York can see the Health and Wellbeing page for other sources of formal support.
For staff at the University of York, please see the Support, Welfare and Health pages.
If you or someone you are concerned about is in crisis now, call 999. Other useful contacts if you are in crisis include the Samaritans (tel: 116 123) or the text service SHOUT (text: 85258).
Further reading
by University of York alumnus Lucy Foulkes
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.

Professor Dean McMillan
Dean has a joint appointment between Hull York Medical School and the Department of Health Sciences, University of York. He is a clinical psychologist with research interests in the development and evaluation of brief psychological interventions for common mental health problems.

Della Bailey
Della developed her clinical career within both the voluntary sector and the NHS. She currently delivers collaborative care and provides supervision to practitioners within the CASPER trial as well as developing materials for use by participants.

Professor Carolyn Chew-Graham
Carolyn is a visiting Professor at the University of York, and Professor of General Practice Research at Keele University.

Professor David Ekers
David is a nurse leader with over 30 years' experience in mental health. For the past 15 years he has operated as a senior Nurse Consultant in Tees, Esk and Wear Valleys NHS Foundation Trust combining clinical, research and leadership roles.

Professor Simon Gilbody
Simon is Director of the Mental Health & Addictions Research Group (MHARG) at the University of York, and holds a joint appointment with the Hull York Medical School (HYMS), where he is a member of the Centre for Health and Population Sciences.

Dr Liz Littlewood
Liz completed her PhD in Psychology at the University of York in 2007, she took up her current post in adult mental health and clinical trials research at the Department of Health Sciences in 2011.
Explore more research
A research project needed to spot trees on historic ordnance survey maps, so colleagues in computer science found a solution.

We’re using gaming technology to ensure prospective teachers are fully prepared for their careers.

A low cost, high-accuracy device, could play a large part in the NHS's 'virtual wards'.
