How social inequality is adding to England's A&E crisis
-
Research
- Health and Wellbeing
- Justice and Equality
Posted on 27 January 2016
Research by our health economists lays bare, for the first time, how inequality is driving an increase in emergency hospital admissions across England

Reducing healthcare inequality is a matter of social justice – but with increasing pressure on A&E services, it’s also a matter of common sense”
People living in some of England’s poorest communities are nearly two and half times more likely than their better-off neighbours to have a preventable emergency admission to hospital.
And it’s not just the poor – people in the middle fifth of neighbourhoods are nearly 50 per cent more likely to find themselves in A&E than those living in the most affluent areas.
Research by our health economists shows this social inequality is increasing pressure on our already over-stretched emergency departments.
Co-ordinated care
Previous studies have shown that many emergency hospital admissions could be prevented by GPs, nurses and hospital staff working more closely together to deliver proactive co-ordinated care – and this is already a key government policy objective.
What this latest research uncovers is the link between emergency admissions and inequality.
“And that link turns out to be strikingly large and important,” says Professor Cookson who led the research. “Our findings suggest that NHS staff will need to pay closer attention to healthcare inequalities in their area if they are to succeed in delivering proactive co-ordinated care to those who need it most.”
He added: “In England, the richest fifth of people can expect to live at least 12 more healthy years than the poorest fifth. One consequence is that poorer people have a lot of preventable illness, which is putting huge pressure on the health service.”
Long-term conditions
The study focused on emergency hospitalisation for patients with long-term conditions such as heart and lung disease, dementia and diabetes.
It showed that nearly half of emergency admissions are attributable to social inequality. The researchers calculated that inequality gave rise to more than 158,000 preventable emergency hospitalisations in the year 2011/12 and nearly 38,000 deaths from treatable conditions.
A new approach
Professor Cookson says a new approach is needed to ease demand for emergency services.
“The NHS is good at providing equal access to GPs and hospitals when people suffer a health emergency. It’s not so good at providing care to people before they suffer an emergency.”
Alongside improved co-ordination of local health services, he is calling for improved information about local healthcare needs. In the wake of the study, a group of academics, led by our Centre for Health Economics, developed a monitoring system based on eight indicators of healthcare inequality which could be used to shape future health service planning.
“To co-ordinate care effectively, NHS managers will need better information about healthcare inequalities in their local area,” says Professor Cookson. “Co-ordinated care sometimes requires paying closer attention to the less well-off, as advantaged people are often better able to care for themselves.
“They have better information, better support networks from family and friends, nicer home environments in which to recover from illness – and sharper elbows.”
Better information, he says, will help healthcare professionals identify who is at risk of preventable hospital admissions and follow them up.
Learning lessons
For example, patients at risk of repeated admissions for breathing difficulties may need follow-up care to make sure they are taking their medicines. Better information will also reveal which local NHS areas are doing well or badly at tackling healthcare inequalities, allowing lessons to be learned.
Wider action is also needed, beyond the NHS.
“Reduced consumption of tobacco, alcohol and sugar would help. But we also need to look at child poverty and early years education because a poor start in life can lead to lifelong inequalities in health. The need for wider government action on social inequality is not an excuse for inaction by the NHS on healthcare inequality."
Professor Cookson added: “Reducing healthcare inequality is a matter of social justice – but with increasing pressure on A&E services, it’s also a matter of common sense.”
Professor Cookson's research was funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research (HS&DR) Programme
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.

Professor Richard Cookson
Professor Cookson's research focuses on equity in health and health care
Discover the Details
How a universal health system reduces inequalities: lessons from England was published in the Journal of Epidemiology and Community Health
England's A&E crisis is fuelled by inequality was published in The Conversation
Find out more about our research on developing NHS equity indicators
Explore more research
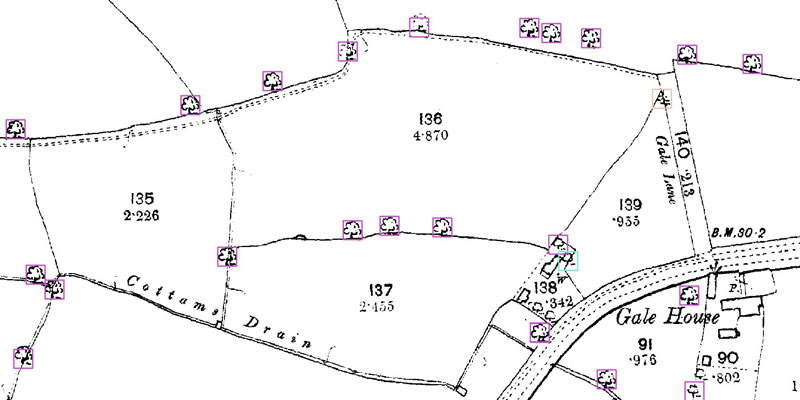
A research project needed to spot trees on historic ordnance survey maps, so colleagues in computer science found a solution.

We’re using gaming technology to ensure prospective teachers are fully prepared for their careers.

A low cost, high-accuracy device, could play a large part in the NHS's 'virtual wards'.
