Hidden agendas: the complicated criteria behind the detainment of offenders with severe personality disorders
Posted on 13 February 2019
Our research is seeking to understand the broad and complex motivations behind the detainment and treatment of dangerous offenders with personality disorders.

When I first came to this subject I thought it was a terrible way of trying to keep people locked up without anyone having an idea of whether they really posed a risk. But over the course of my research I found there are many opinions, and I wanted to show their side of the story.
When launching criminal justice policies, governments often talk about a desire to protect the public, and their determination to be ‘tough on crime’. Such media-friendly mantras may help to win votes, but the reality behind the launch of a new policy is frequently complicated, sometimes controversial, and unlikely to win over the press.
Dr Ailbhe O'Loughlin from our Law School has published a paper focusing on the Dangerous and Severe Personality Disorder (DSPD) Programme, an initiative which was claimed to both protect the public, and give offenders with disorders thought to be untreatable the chance of rehabilitation through newly devised therapies.
Background
She explains the background to the programme: "Prior to 2007, mental health legislation made it difficult to detain people with personality disorders who were thought to pose a risk to the public, because there was a requirement for two psychiatrists to certify that the person they were detaining was treatable."
She said differences in opinion as to whether people with personality disorders - particularly anti-social disorders - could be treated, meant a trend developed toward hospitals refusing to take these sort of patients for fear the practice was unethical.
“Some in the medical profession saw themselves as complicit in keeping people nearing the end of their prison sentence locked up in hospitals because there was no other way of detaining them,” said Dr O’Loughlin.
Controversial
This was controversial: it appeared to be a means of locking people up beyond the length of their sentence, even if there was little evidence they would benefit from treatment in hospital.
Spurred on by several high profile cases in the 1990s of violent offenders being released from prison, and murders by psychiatric patients, the new Labour government came to office determined take a new approach to the issue, and proposed changes in the law to deal with this group of offenders.
“They proposed amending the Mental Health Act 1983 to remove the requirement of treatability, thus removing the barrier to detention,” says Dr O’Loughlin. “They also proposed to create a new form of detention on the basis the patient was dangerous and had a severe personality disorder.”
But this too was controversial. In legal terms, defining exactly what ‘dangerous’ is can be less than straightforward, and there was concern that people would be detained on the strength of what they might do in the future, not what they had done in the past; a practice seen by many as an affront to civil liberties.
Dangerous
And to further complicate the situation, Dr O’Loughlin says debates in parliament on a new Mental Health Bill became focused on the fear of ‘dangerous people’, and an opportunity to introduce progressive mental health legislation based on improving patients’ access to treatment was missed.
“The debate went down a very risk and danger focused route, and making it easier to detain people,” she says.
Against this politicised background, and despite some dissenting voices, the DSPD programme commenced. New treatments and risk prediction tools were funded, hospital and prison units were set up and a pilot ran for some ten years. But the research wasn’t without its critics.
“There was criticism at the time that the research wasn’t systematic,” says Dr O’Loughlin. “Researchers often used different approaches, there was no control group and no way of determining whether treatments were effective in a robust scientific way.”
So she was surprised when, in 2011, the coalition government expanded the DSPD programme and she began to explore whether there might be other reasons to keep the programme alive.
Research
She says research evidence stretching back as far as the 1970s showed that patients with personality disorders not only presented problems for the public, but were challenging for the institutions which housed them. It began to look as though the DSPD programme was as much about enabling easier management of patients, as it was protecting the public.
“If a person was self-harming or violent they were managed by being moved from prison to prison, or segregated, meaning they would get very little help for their personality disorder,” says Dr O’Loughlin.
“In psychiatric hospitals patients might cause problems by manipulating staff or other patients, and some were excluded from treatment for fear this might create more opportunities to manipulate the system.”
Dr O’Loughlin believes dealing with this situation became one of the objectives of the DSPD programme.
“I think part of the reason the programme was created was to find a way of bringing these particular patients into the mainstream and treating them in a more ‘routine’ way in prisons; ie engaging in rehabilitation, moving down through the security categories, and eventually being released,” she says.
In short, the programme made prisoners easier to manage, reducing the risk they posed within the prisons themselves and so aiding the management of the institution.
Appreciation
But Dr O’Loughlin stresses that as her research developed, her appreciation for the differing opinions of those working in the area grew.
“When I first came to this subject I thought it was a terrible way of trying to keep people locked up without anyone having an idea of whether they really posed a risk. But over the course of my research I found there are many opinions, and I wanted to show their side of the story.
“Although policy makers may appear to focus on protecting the public and offering the offender a chance of rehabilitation, the reality is this group of personality disordered offenders pose a myriad of risks - to the public, themselves, the institution housing them, staff, other patients, the reputation of the government of the day, and the mental health system itself. So you can’t understand what the programme is doing or how it came about unless you pay attention to that.”
And she hopes this paper may play a part in assisting any changes in policy in future.
“If you want to change a system, you need to fully understand it and the motivations behind it, and that’s what this paper aims to enable,” she says.
“Once you have a better idea of what’s going on you can start to look at how things could be different or how they can be improved.”
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.

Dr Ailbhe O'Loughlin
Research Title: Lecturer
Ailbhe's research interests include the role of risk and risk assessment in criminal justice and mental health law
Explore more research
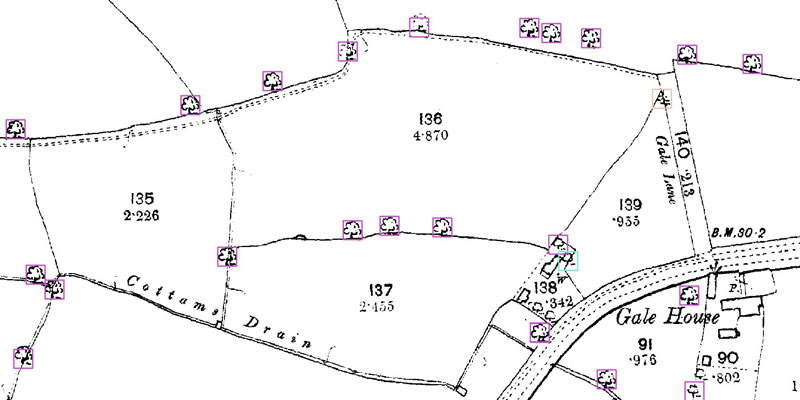
A research project needed to spot trees on historic ordnance survey maps, so colleagues in computer science found a solution.

We’re using gaming technology to ensure prospective teachers are fully prepared for their careers.

A low cost, high-accuracy device, could play a large part in the NHS's 'virtual wards'.
