What are the ongoing health risks for survivors of childhood cancer?
We tracked survivors of childhood ALL through their teenage and young adult years to see how their health fared

Background
Accounting for around 40% of all cancers diagnosed in children before the age of 15, Acute Lymphoblastic Leukaemia (ALL) is the commonest childhood cancer. We tracked survivors of childhood ALL through their teenage and young adult years to see how their health fared. Involving most clinical specialties, we found that hospital attendances were much higher than expected, and that ALL survivors were more than twice as likely as their unaffected counterparts to fall under the care of endocrinology, cardiology, neurology, ophthalmology or respiratory medicine. These large differences continued over the 25 years of the study with no sign of declining.
This information shows how important it is for doctors and patients to take a previous diagnosis of childhood ALL into account when assessing seemingly unrelated health problems in later life.
Patterns of ill health
Confirming the well-known observation that some ALL survivors experience later health problems, our research was able to look in greater detail at key health indicators. Adding substantially to existing knowledge, we analysed hospital inpatient and outpatient records, examining visits to individual clinical specialties and monitoring how these visit patterns changed over time.
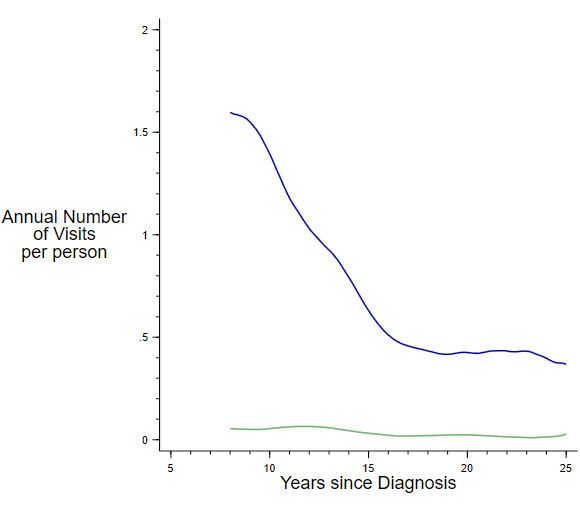
Childhood ALL survivors are routinely monitored in outpatient clinics run by paediatricians, haematologists and/or oncologists. As shown in Figure 1 below, the frequency of this monitoring falls over time (blue line), although never quite reaches the low level seen among individuals of the same age and sex in the general population (green line).
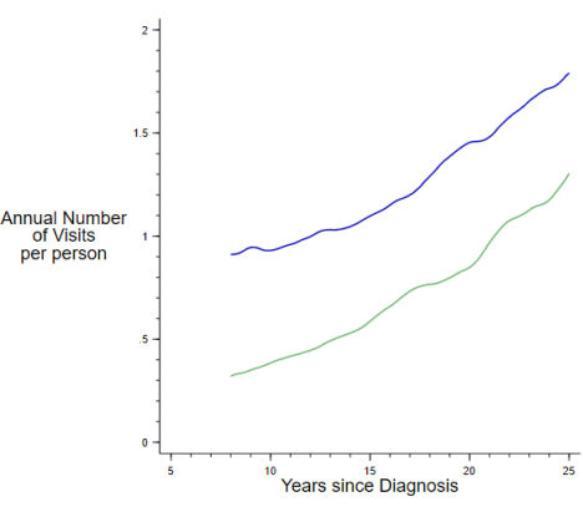
By contrast, as can be seen in Figure 2 below, visits to outpatient clinics run by doctors in other clinical specialties, increased over time; with ALL survivors (blue line) visiting consistently more often across the 25 years than their general population counterparts (green line).
Which types of health conditions?
When we look more closely at which clinical specialties survivors visited, we see that ALL survivors are far more likely than their peers to visit nearly all specialties. Figure 3 shows the seven specialties where the largest differences were found. In both males and females, the biggest disparity is seen for endocrinology, which over 25% of survivors attended on at least two occasions compared to less than 2% of the general population. Notable differences also occur for cardiology, neurology, ophthalmology, respiratory medicine and general medicine.
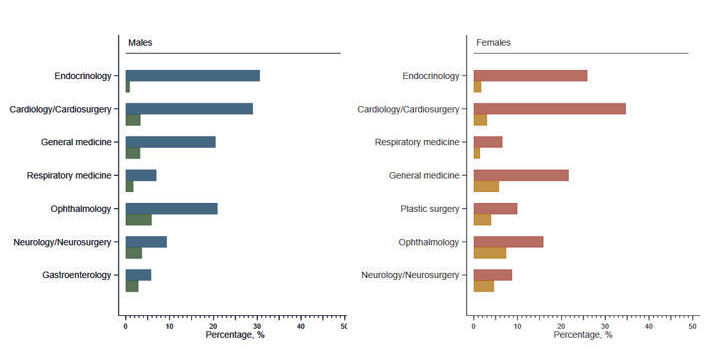
Figure 3: Percentage of survivors of childhood ALL (males: blue; females: red) who attended different outpatient specialties, compared to the general population (males: green; females: orange).
Dr Sally Kinsey, the consultant paediatric haematologist involved in this research, explains further:
"Problems that result from chemotherapy and radiation treatment can include: impacts on fertility, cataract formation, hormonal problems including underactive thyroid gland, and nervous system problems, rarely including brain tumours (often benign).
As many of these problems occur several years after the end of treatment for ALL during young adulthood, GP referrals to specialist hospital services may not mention the previous ALL diagnosis and treatment. As a result, some of the late-effects of cancer treatment as a child may not be considered, but actually are the root of the problem. So, it is important that the young people are made aware of the potential for their past ALL treatment being involved in their current illness and can discuss this at their hospital appointments when referred. Hopefully leading to faster diagnosis and treatment.“
Different types of treatment for ALL
The ALL patients in this study were from an era when treatment could be particularly toxic and routine cranial irradiation was used (1992-1996). After this time, some of these treatments were withdrawn, and others were used less frequently. Nowadays, cranial irradiation is used sparingly, and children with ALL are regularly tested to see how they are responding to treatment. This means that in the future, the present study can be used to evaluate the impact of these more recent changes on the longer-term health of childhood ALL survivors.
The significance of the research
Professor Eve Roman, who led this research, comments on its significance for ALL survivors:
“Epitomising one of the major therapeutic success stories of the last 50 years, 5-year survival for childhood ALL is now around 90% in high-income countries like the UK. As a result, the numbers of childhood cancer survivors is increasing year-on-year. Whilst the health of those who are cured of cancer may return to normal, some survivors go on to develop longer-term health problems. As such, the striking findings presented in this report underscore the need for clinicians and patients to take a previous diagnosis of ALL into account when interpreting seemingly unrelated symptoms in later life.”
Read the full research
A note on how we undertook the research
Data are from the United Kingdom Childhood Cancer Study (UKCCS), a national population-based study established in the 1990s to investigate potential causes of childhood cancer. Each child with cancer (cases) was matched with two children of the same age and sex who didn’t have cancer (controls). These children’s health is now being tracked by linking to nationwide information on inpatient admissions and outpatient attendances as well as cancers and deaths, should such events happen. This research reports findings for 1,082 children diagnosed with ALL in England who survived for at least 5 years, and 2,018 controls.
Our findings are based upon linked hospital data recorded when the patient visited hospital; so data are available for everyone in the study over the whole 25 years and this completeness means that there is no missing information for either survivors or their general population counterparts. Data from other healthcare services outside the hospital setting were not available, so importantly we were not able to examine how often childhood cancer survivors access primary care and adolescent psychosocial services.
Contact us
Helen Cohen
ECSG Research Administrator
helen.cohen@york.ac.uk
+44 (0)1904 32 1927
Seebohm Rowntree Building,
University of York,
UK,
YO10 5DD
Twitter
Related links
Read the full research article here:
Excess morbidity and mortality among survivors of childhood acute lymphoblastic leukaemia
Contact us
Helen Cohen
ECSG Research Administrator
helen.cohen@york.ac.uk
+44 (0)1904 32 1927
Seebohm Rowntree Building,
University of York,
UK,
YO10 5DD
Twitter
Related links
Read the full research article here:
Excess morbidity and mortality among survivors of childhood acute lymphoblastic leukaemia