“The health service has many competing interest groups and pressures and we provide evidence to inform the debate,” said Professor Andrew Street, a frequent commentator in the national media and an authority on productivity and payment in the NHS.
“Health economics provides the tools and insights to make the health service better by aligning spending decisions to patient outcomes,” he added. To be effective, Professor Street and his team at the Centre for Health Economics, require the free flow of accurate and reliable information from the NHS. But that is not always available.
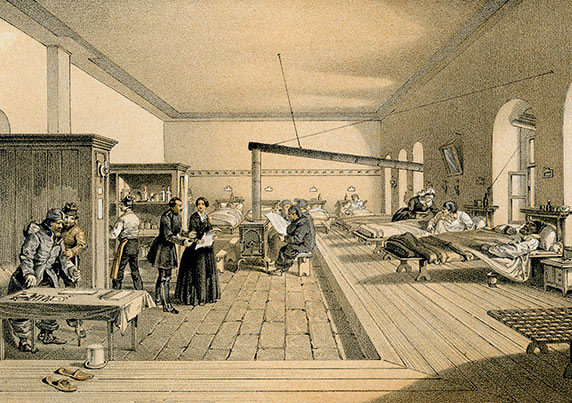
In a recent lecture, Realising Florence Nightingale’s Vision, Professor Street showed that key data on how patients feel about their care, and the effect it has on their wellbeing, have been suppressed or simply unavailable for much of the last 150 years.
Listening to patients
“Florence Nightingale understood the importance of listening to patients and collecting this information back in the nineteenth century,” he said. But the Royal Colleges at the time had other ideas: they suppressed publication and even the collection of such data. Even today, he said: “For the vast majority of people who use the health service we don’t routinely collect information about whether they get better or not. This makes it impossible to assess how well the NHS is fulfilling its primary function of improving the health of the nation.”
But attitudes are changing, he says, with the NHS becoming progressively more patient-focused. As patients have become more assertive over recent years, English health care professionals have begun to listen to patients and collect the data not only about what treatments they receive but also the outcomes they experience. “We are able to use the data to get a better understanding of the quality of care and its impact on health” he said.
https://soundcloud.com/university-of-york/andrew-street-why-we-should-listen-to-patients
Patient outcomes
The Centre for Health Economics has been at the forefront of developing ways of collecting information about patient outcomes, and in using this information to evaluate different treatments and the health system as a whole.
Professor Street’s analysis of productivity and performance within the NHS sets benchmark standards by which the efficient delivery of healthcare is measured. His work builds on the foundations laid by Florence Nightingale, who believed that is was impossible to improve the health service without information about what happens to the people who use it.
“Decisions about the health system should not be made by lobbyists and those with vested interests. The best way to resist the lobbyists is to have information about how the NHS serves the people that use it, so that decisions can be based on evidence, not opinion. Our work is designed to contribute to this evidence-base.,” he said.
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.