The issue
Obesity and the rising incidence of type 2 diabetes is a major healthcare concern worldwide and has been a focus of activity amongst pharmaceutical companies striving to introduce new drugs. Any new drugs not only undergo rigorous safety checks, but careful clinical trials are conducted to study efficacy and monitor side effects in humans. A correct interpretation can require an in-depth understanding of both how a drug works and of the mechanism behind any incidental side effects, but this may be difficult to achieve when simple and/or non-human experimental platforms are used. Bladder cancer is among the top 10 most common cancer types in the world, with approximately 550,000 new cases annually. Bladder cancer typically receives less funding for research than the other common cancer types and although smoking is commonly cited as the main risk, there is still much that remains to be understood.
The research
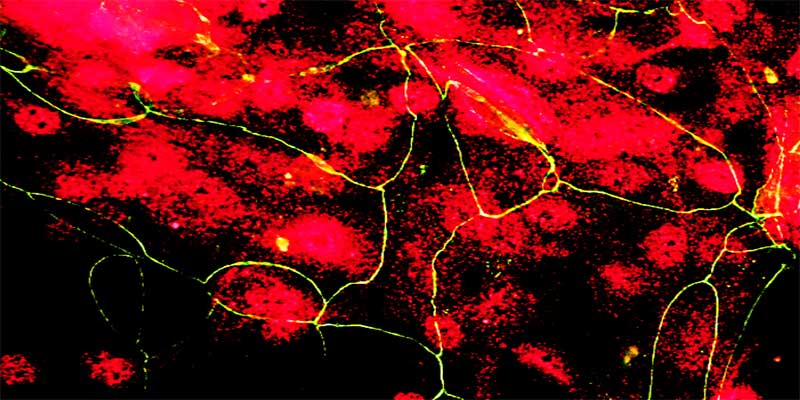
The Jack Birch Unit (JBU) focuses on human urinary tract cancers, including bladder cancer. The JBU’s core philosophy is that in order to understand cancer, it is essential to build this on a detailed understanding of the normal human cell and tissue biology. To do this, the JBU has developed an experimental approach where normal human urothelial cells are isolated from surgical samples and propagated as normal cell lines in vitro. Investigations conducted in the JBU back in the early 2000s focussed on a particular nuclear receptor, peroxisome proliferator-activated receptor gamma (PPARgamma), and demonstrated for the first time a direct link between the complex pathways regulating proliferation versus the specialisation of urothelial cells to form a urinary barrier. Synthetic compounds of the thiazolidinedione (TZD) class, including troglitazone and rosiglitazone, are known to be able to activate PPARgamma and both were used experimentally to induce urothelial differentiation.
The outcome
Not only is PPARgamma implicated in urothelial cell proliferation and differentiation, but other researchers had shown it to be involved in the development of fat cells through the process of adipogenesis. In 2004, multiple pharmaceutical companies were developing drug compounds to activate PPARs for the treatment of type 2 diabetes and metabolic syndrome. Of particular concern were dual specificity PPAR ligands, which are compounds that activate both PPARgamma as well as its highly-related family member PPARalpha. Animal trials with dual specificity PPARalpha+gamma agonists led to significant concerns about their use in Europe and the USA, due to the development of bladder cancer. The JBU worked collaboratively with one company (Novo Nordisk) to understand how dual PPAR agonists caused cancer and to determine the relevance to human bladder carcinogenesis. This work was important because it disputed other theories that argued rodent bladder carcinogenesis by PPAR dual agonists was not of human relevance. The work was used in a landmark trial about Actos (a PPARgamma-selective drug with alpha activity) and bladder cancer.