The issue
Devised with the overarching aim of overcoming existing limitations and providing functional, generalisable data to inform contemporary clinical practice and research, the UK’s Haematological Malignancy Research Network (HMRN) was established at the University of York by ECSG researchers and NHS clinicians in 2004.
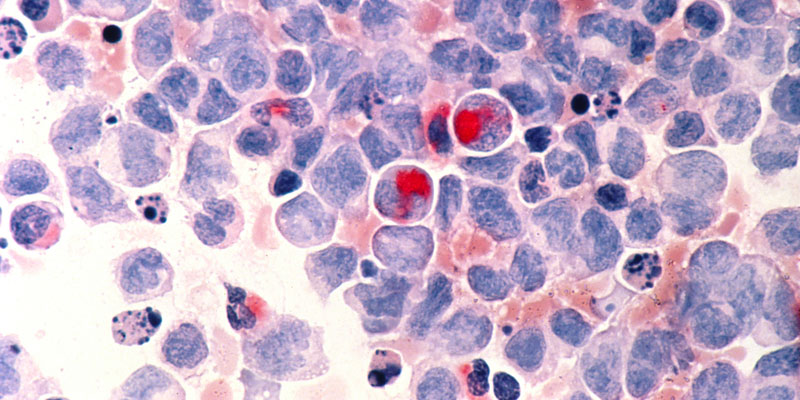
The World Health Organization's 2001 classification of tumours of haematopoietic and lymphoid tissues, which defined over 100 subtypes, has been rapidly adopted into clinical practice.
However, the classification posed significant challenges for national cancer registries. Many have struggled to capture the data required for implementation, and are continuing to report using historical groupings that have no relevance to modern clinical practice, commissioners, patients, or researchers.
The problem has been recognised by the National Institute for Health and Care Excellence (NICE), which commented: “There are no precise and reliable figures for incidence and survival rates for the different forms of haematological cancers in England and Wales."
The European Cancer Registry (EUROCARE ) also noted the issues, stating that “the evolving classification and poor standardization of data collected on haematological malignancies vitiate the comparisons of disease incidence and survival over time and across regions."
The research
Devised with the overarching aim of overcoming existing limitations and providing functional, generalisable data to inform contemporary clinical practice and research, the UK’s Haematological Malignancy Research Network (HMRN) was established at the University of York by researchers and NHS clinicians in 2004.
With centralised diagnostics covering a unified clinical network, HMRN’s catchment population of ~4 million in 14 hospitals has a similar socio-demographic structure to the UK as a whole.
Capturing biological, clinical, treatment and outcome data on all patients with pathologically conformed haematological malignancies (irrespective of age, prognosis and treatment intent) to clinical trial standards, HMRN operates on a legal basis that permits all patients to be followed through local and national NHS systems until death, regardless of consent.
The outcome
HMRN’s maturing longitudinal data, coupled with its capacity to adapt to changing diagnostic and treatment categorisations, provides an unparalleled, real-world contemporary resource to address emergent questions of concern to researchers, clinicians, commissioners and regulators, policymakers and patients.
Population-based data is required not only to inform aetiological hypotheses and plan healthcare services, but also to monitor the impact of therapeutic change in the general patient population.
This need is particularly pertinent in fast-moving areas like haemato-oncology where treatment protocols are subject to rapid change, and trials are restricted to specific patient groups (usually common subtypes and younger fitter patients).
Accordingly, with research spanning the whole patient pathway, from disease determinants through to diagnosis, treatment and outcome, the ‘real-world’ evidence produced by HMRN also contributes to:
- NHS decision making
- national cancer statistics
- UK clinical guidance and policy decisions
- patient and public information.