Incorporating health inequality concerns into performance monitoring and economic evaluation – feasibility study in colorectal cancer
Overview
The main purpose of this project was to demonstrate that it is feasible to monitor the contribution of the NHS to tackling health inequality in one specific “pilot” area of colorectal cancer.
The project laid the groundwork for future research on developing indicators of NHS performance in a range of cancer services. It has helped build inter-disciplinary collaborative links between economists at the University's Centre for Health Economics (CHE) and cancer epidemology / public health specialists in the Department of Health Sciences and the Leeds Institute for Molecular Medicine. It has also facilitated new inter-disciplinary and cross-institutional networking between health economists in CHE and public health experts, in particular, at UCL, University of Manchester, and University of Newcastle.
Prelimimary findings from this pilot study were presented as a poster at the National Cancer Intelligence Network Conference in Brighton in June 2013. The intention is to translate future findings into practice by developing "equity dashboards" for NHS decision makers in NHS England and Clinical Commissioning Groups, as part of the follow-on three year project on developing NHS equity performance indicators.
In detail
The main purpose of this project was to demonstrate that it is feasible to monitor the contribution of the NHS to tackling health inequality in one specific “pilot” area of colorectal cancer.
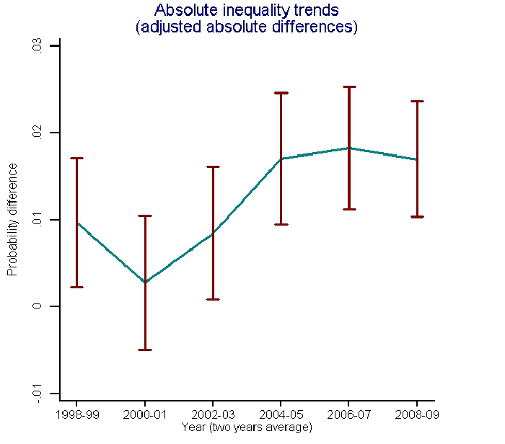
Hospital episode statistics were used to examine five outcomes for patients undergoing primary colorectal cancer surgery in the English NHS for twelve financial years 1998/9 to 2009/10. The researchers described unadjusted two-year trends by quintile groups of English small area income deprivation, and estimated absolute and relative inequality gaps between most and least deprived groups after adjusting for age, sex and co-morbidity.
Preliminary findings were that inequality reduced for one indicator (abdominoperineal resection in rectal cancer surgery), increased for one indicator (open versus laparoscopic surgery in colorectal cancer surgery), and remained approximately stable for the other three (28-day in-hospital mortality, 30-day emergency re-admission and length of stay for colorectal cancer surgery). Abdominoperineal resection in rectal surgery fell more rapidly among deprived groups (from around 30% to just under 20%), with an initial absolute inequality gap of 10 percentage points falling to 5 by 2004-6. Laparoscopic surgery rates increased more rapidly among affluent groups (from zero to 30%), with an initial inequality gap of zero rising to four percentage points in 2008-10. 28-day in-hospital mortality fell at a similar rate in all groups, with an absolute inequality gap of about one and a half percentage points throughout except for a reduction to a half percentage point gap in the two year period 2000-1. Length of stay fell at similar rates in all social groups, with an absolute gap of approximately two days throughout. 30-day emergency re-admissions increased at a similar rate in all groups, with an absolute gap of about one percentage point throughout.
The project has laid the groundwork for future research on developing indicators of NHS performance in a range of cancer services (not just bowel cancer). It has helped build inter-disciplinary collaborative links between economists at the University's Centre for Health Economics (CHE) and cancer epidemology / public health specialists in the Department of Health Sciences and the Leeds Institute for Molecular Medicine. It has also facilitated new inter-disciplinary and cross-institutional networking between health economists in CHE and public health experts, in particular, at UCL, University of Manchester, and University of Newcastle, in preparation for further grant bids. This networking has already resulted in a successful cross-institutional grant bid to NIHR HSR&D programme for a three year project to develop indicators of NHS equity performance from Jan 2013 to Dec 2015, as well as further proposals under development.
Prelimimary findings from this pilot study are being presented as a poster at the National Cancer Intelligence Network Conference in Brighton in June 2013. The intention is to translate future findings into practice by developing "equity dashboards" for NHS decision makers in NHS England and Clinical Commissioning Groups, as part of the follow-on three year project on developing NHS equity performance indicators.
Outputs
Grants
- Richard Cookson, NIHR, Developing indicators of change in NHS equity performance, £493,638
Principal Investigator
Dr Richard Cookson
Centre for Health Economics
richard.cookson@york.ac.ukCo-Investigators
Dr Steven Oliver
Health Sciences/HYMS
steven.oliver@york.ac.uk
