Older People
This section showcases projects that focus on people aged 65 and over. We are adding new studies to this section every few months, so please keep checking in to keep up-to-date.
The 95+ Study
Project title
Identity Construction in the Very Old: A qualitative narrative study
What we did
As people grow older, the way they see themselves, how they behave and how they interact with others, can change. In this study we investigated how people aged over 95 years hold on to their sense of identity and continue to negotiate their place in society.
According to the 2021 Census, 609,000 people in the UK are aged 90 years or more. Typically, society sees ageing as a period of decline and withdrawal from society. Despite this, there is little research on how older people see themselves.
We interviewed 23 people in the North East of England who were aged over 95 years. We asked about their day-to-day life, health and thoughts about the future.
Five themes were generated from the interviews: Contentment; Independence; Family roles; Keeping up appearances; Reframing ill health.
We found that striving for independence sometimes meant risk-taking and resistance because this was preferable to losing autonomy. This might help us rethink how very old people in society view safety and risk and the tensions this may cause with those who provide care. Ultimately, we ought to question whether we should work to achieve a better balance between surviving and thriving.
How we did it
A qualitative interview study was designed to gain participants’ perspectives and experiences of living life as the very old in society and the resulting challenges and advantages, set within the context of their individual biographies. We aimed to explore, through a Positioning Theory lens, how self-concept and identity is experienced.
Interview data were generated through qualitative interviews with people aged between 97–99 years old (n = 23). Participants were purposively sampled from the 80 remaining participants in a 10 year follow up study to The Newcastle 85+ Study which was a longitudinal observational cohort study of people born in 1921 and who were registered with Newcastle upon Tyne or North Tyneside Primary Care Trusts in the UK in 2006. Sampling attempted to ensure variation within the confines of the study population: gender (female n = 16, male n = 7); stated place of residence; morbidity and frailty. Participants had a range of health and social care needs and different levels of support from family and friends.

Research Inclusion: People 95 years and over
Despite the increased number of people reaching very old age, experiences of the very old in society are rarely researched and how they negotiate their sense of self in their world as they age is little understood.
Our study focused on participants aged over 95 years. It is one of very few studies focusing of this age group. The aim was to give voice to, and gain understanding of, how some of the oldest people in society conceptualise their identity and negotiate their continued place in the world.
Team
The team was comprised of a multi-disciplinary group of researchers from the University of York and Newcastle University
Funder information
National Institute for Health and Care Research (NIHR) Research for Patient Benefit (PB-PG-1217_200025)
The CASCADE study
Project title
Case finding for depression in primary care: a regression discontinuity design (CASCADE)
What we did
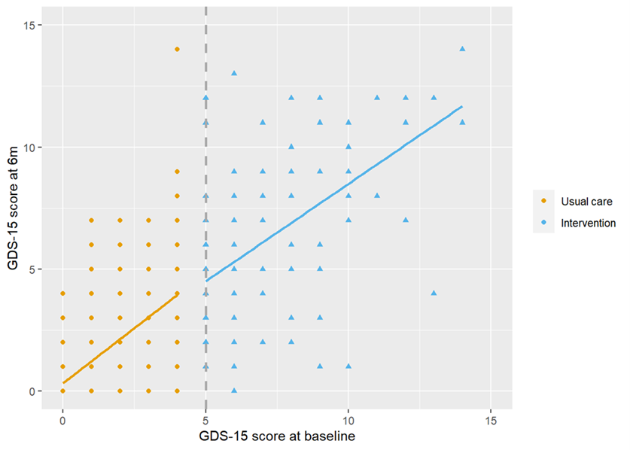
Depression is the most common mental health disorder amongst the older population, but the majority of people do not receive help from the NHS. There is little evidence that screening older adults for depression is effective and cost-effective at reducing depressive symptoms. The aim of the CASCADE study was to replicate this work to ascertain whether screening older adults using the Geriatric Depression Scale and alerting them and their GP if their response indicated symptoms of depression was associated with an improved GDS-15 score six months later.
We undertook a regression discontinuity study with an embedded health economic analysis and qualitative study. If answers indicated that a participant might be depressed, we let them and their GP know, so they could take action. Participants completed our questionnaire again six months later. We then checked whether their symptoms of depression had decreased.
We found a very small decrease in participants' depression scores after six months, among those with depressive symptoms. This wasn't enough to say that screening was helpful or that the additional cost of screening would be value for money for the NHS.
How we did it
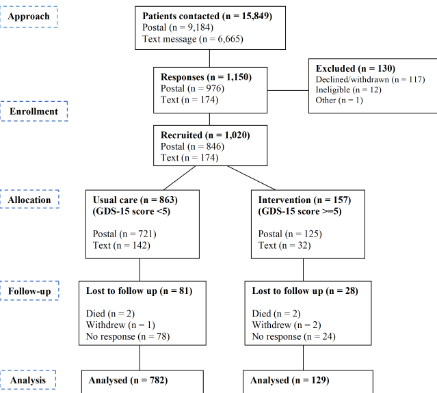
We contacted 15,849 patients from 15 GP practices in the north of England;1020 people over 65 years of age, living in the community, who had not been diagnosed with depression took part. Based on GDS-15 scores, we assigned patients to two groups: usual care (scores of 0-4) or intervention (scores of 5+). We used regression discontinuity analysis to explore whether GDS-15 scores differed between these groups 6 months later. We also interviewed patients and health care professionals involved in delivering the intervention. The data were thematically analysed to gauge acceptability of the intervention, to understand the processes of delivering the intervention, and whether it should continue post study completion. A cost-utility analysis was undertaken to explore the impact of screening followed by alerting patients and GP on costs and health-related quality of life.
We concluded that it is unlikely that the screening method used in our study will help people with depression feel better after six months.
Research inclusion: People 65 years and over
We included 1020 people over the age of 65 years in the study. To our knowledge, this is the first prospective RD evaluating the effectiveness of the GDS to screen older patients for depression. A PPI member was part of the independent Trial Steering and Data Monitoring Committee. This ensured that patients were represented on the panel and their views fed into core study decisions.
Team
The CASCADE research team at the York Trials Unit, University of York, was led by Professor David Torgerson and Caroline Fairhurst, and included expertise in methodology (David Torgerson), statistical analysis (Caroline Fairhurst, Kalpita Baird, Jennie Lister), study management (Sarah Cockayne, Dr Rachel Cunningham-Burley, Dr Laura Clark, Ailish Byrne), health economics (Dr Kerry Bell, Qian Zhao) and qualitative research (Professor Joy Adamson, Helen Anderson). Additionally, Professor David Ekers (Tees, Esk and Wear Valleys NHS Foundation Trust) contributed expert clinical advice.
Find out more on the study website:
https://www.york.ac.uk/healthsciences/research/trials/ytutrialsandstudies/archive/cascade/
Funder information
The research was funded by National Institute for Health and Care Research (NIHR) Research for Patient Benefit (Grant Reference Number NIHR203506).
The OTIS study
Project title
Home environmental assessments and modification delivered by occupational therapists to reduce falls in people aged 65 years and over: the OTIS RCT
What we did
Falls and fall-related fractures are highly prevalent among older people and are a major contributor to morbidity and costs to individuals and society. We conducted a randomised controlled trial to determine the clinical and cost-effectiveness of a home hazard assessment and environmental modification delivered by occupational therapists for preventing falls among community-dwelling people aged ≥ 65 years who are at risk of falling.
In total, 1331 participants were randomised (intervention group, n = 430; usual-care group, n = 901) and followed up for 12 months. Participants were asked to complete and return monthly falls calendars to report if and when they fell. All participants received a falls prevention leaflet and routine care from their general practitioner. The intervention group were additionally offered one home environmental assessment and modifications recommended or provided to identify and manage personal fall-related hazards, delivered by an occupational therapist. The primary outcome was the number of falls per participant over the 12-month follow-up.
The intervention was not seen to be effective, with an increase in fall rate in the intervention group relative to usual care (adjusted incidence rate ratio 1.17, 95% confidence interval 0.99 to 1.38; p = 0.07).
Consequently, we do not recommend occupational therapist-led home assessment for patients who have characteristics similar to those of patients included in our study. Scarce occupational therapist resources would be better employed elsewhere.
How we did it
We undertook a pragmatic, two-arm modified cohort randomised controlled trial in eight NHS trusts in primary and secondary care in England. In total, 1331 participants were randomised in a 2:1 allocation to either usual care plus a falls prevention leaflet or to receive the home hazard assessment and environmental modification intervention, plus usual care and a falls prevention leaflet. The primary outcome was the number of falls per participant over the 12 months from randomisation. Secondary outcomes included; proportion of fallers and multiple fallers, time to fall, and fear of falling.
Research inclusion: People aged 65 years and over
Falling is a common problem among older people. In fact, up to half of people aged over 80 years fall each year, with most falls happening inside the home. Unfortunately, some falls cause serious injuries, such as broken bones. People often think that falls are part of getting older and that little can be done to stop them from falling. However, there are many ways to reduce falls. The Occupational Therapist Intervention Study (OTIS) explored whether or not a home assessment visit by an NHS occupational therapist could reduce falls among older people who are likely to be at risk of falling.
We included 1331 participants over the age of 65 years in the trial. In addition, OTIS was informed throughout by the involvement of older people with a history of falls. Patient and public representatives were identified from the cohort of participants who had taken part in previous studies led by the study team. The group consisted of four older people.
Team
The OTIS research team comprised a multi-disciplinary and international group of researchers, including from York Trials Unit (University of York, UK), James Cook University (Queensland, Australia), Leicestershire Partnership NHS Trust (UK), University of Nottingham (UK), Institute of Health Research, (University of Exeter, UK), York Teaching Hospital NHS Foundation Trust (UK) and Institute of Population Health Sciences (Queen Mary University of London, UK).
Find out more on the study website:
https://www.york.ac.uk/healthsciences/research/trials/ytutrialsandstudies/archive/otis/
Funder information
This project was funded by the National Institute for Health and Care Research (NIHR) Health Technology Assessment Programme (HTA 14/49/149).
