Impact of early warning systems on patient outcomes
Many in-hospital deaths are predictable and preventable and are often associated with poor clinical monitoring on the ward.
Early warning scoring systems are widely used in hospitals to track patient deterioration and to trigger escalations in clinical monitoring and response.
National adoption of the NEWS system is advocated.
The evidence base for early warning systems is very limited but does suggest potential reductions in cardiac arrests and unplanned ICU admissions.
Substantial resources are being invested in electronic early warning systems across the NHS. Given finite budgets, monitoring of costs, resource use and impact on patient outcomes is crucial to any deployment.
Continuous training and support for ward level staff (including bank nurses) will be integral to system implementation and to longer term maintenance.
Background
Many in-hospital deaths are predictable and preventable and are often associated with poor clinical monitoring on the ward.1 Identifying those patients at risk of clinical deterioration is a major issue for secondary care. NICE guidance recommends that all patients should be monitored to help identify those whose clinical condition is deteriorating or is at risk of deterioration.2
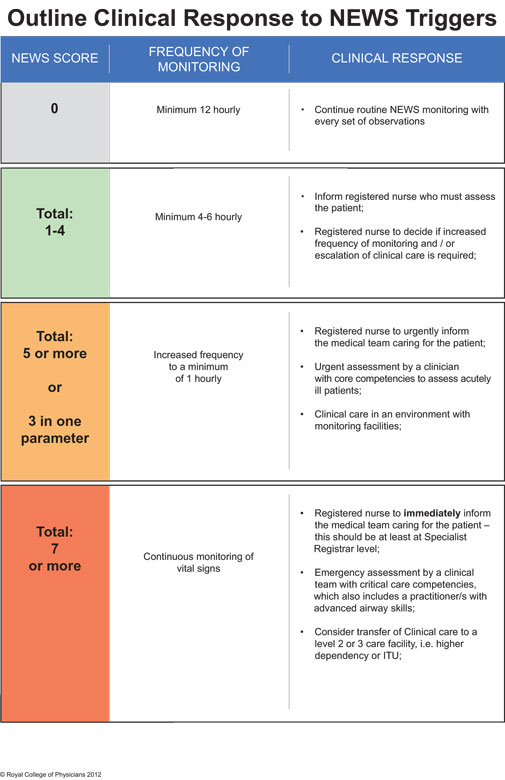
Early warning scoring systems are widely used in hospitals to track patient deterioration and to trigger escalations in clinical monitoring and rapid response by critical care outreach teams. The scoring systems used to trigger escalation are based on routine observations by ward staff. Measurement of physiological parameters of respiratory rate, oxygen saturation levels, blood pressure, temperature, pulse rate and level of consciousness are combined to give weighted scores that in turn trigger graded clinical responses.
A number of aggregate weighted scoring systems are in use. This variation in practice across the UK, has led the Royal College of Physicians to develop a standardised national early warning scoring system known as NEWS.3
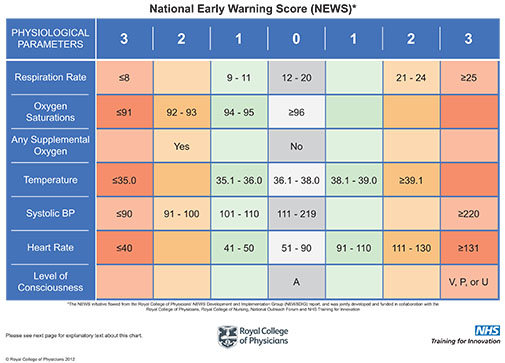
National adoption of NEWS is being widely advocated.4 The aim is to build on existing systems of routine monitoring and standardise the method of assessment of illness severity across the NHS. The outline clinical response for NEWS is presented at the end of this bulletin. The Royal College of Physicians working party recommends that organisation of the clinical response to acute illness should be reviewed and agreed locally.
NHS hospital Trusts implementing early warning systems need to be aware of the extent of evidence supporting their use in routine practice. This issue of Effectiveness Matters summarises evidence from recent systematic reviews that assess whether early warning systems improve patient outcomes compared to standard processes of care. The bulletin has also been informed by roundtable discussions hosted by the Yorkshire and Humber AHSN Improvement Academy.
Effectiveness
The impact on early warning systems on patient outcomes has been subject to systematic review.5-7 The two most recent reviews have some methodological limitations but nevertheless present a good overview of the extent and quality of the available evidence base.6,7
Overall, much of the available evidence is of poor quality.6,7 Most studies employ uncontrolled before and after designs making it difficult to attribute causation and highly likely that any future, better quality research will have an important impact on any estimate of effect. In addition, a wide variety of scoring systems and methods of rapid clinical response have been implemented without adequate control for other potential confounding factors. No formal evaluations of the implementation of NEWS have been published.
From the evidence presented, it appears that NEWS-like aggregate weighted scoring systems perform better than single parameter systems in identifying deteriorating patients.
In relation to patient outcomes, early warning systems when combined with rapid response appear to have the potential to reduce cardiac arrests and unplanned ICU admissions. Impact on reducing in-hospital mortality was mixed. These findings are in line with an earlier review of 18 randomised studies evaluating the deployment of rapid response teams in hospitals.8 This review found that intervention by rapid response teams appeared to reduce rates of cardiac arrest outside the ICU but found no impact on in-hospital deaths.
Although reporting of details on patient populations was very limited, it appears observed effects were apparent in those surgical / high risk patients where deterioration is more predictable.
Accuracy of scoring systems
The accuracy of data recording and the calculation of early warning scores can in turn impact on the accurate detection of patient deterioration. Inaccuracies can lead to delays in identifying patients at risk and or to unnecessary use of health care resources. Considerable investment is being made in either the development of in-house or the acquisition of commercially available electronic systems by NHS Trusts across the NHS. There are some small scale studies that have compared paper versus electronic methods for speed and accuracy.9,10 A more recent study has suggested an association between use of electronic systems and reduced in-hospital mortality.11 However, these are areas yet to be subject to systematic review.
NICE has made a recommendation for research to examine the effectiveness and cost effectiveness of electronic monitoring systems compared with manual recording systems in identifying people at risk of clinical deterioration in general hospital ward settings.2 This is a gap that has yet to be addressed.
Cost effectiveness
No formal evaluations of cost effectiveness of early warning systems (electronic or paper based) were identified. Given finite budgets, there will be opportunity costs attached to the current investment by NHS Trusts in electronic systems. Clear monitoring of costs, resource use and impact on patient outcomes will be crucial to determining whether these systems actually deliver a return on investment.
Implementation issues
A whole systems approach is being advocated for the provision of emergency and acute services across England. Early warning systems and the resulting graded response strategies should therefore be fully integrated into critical and elective care pathways. Electronic warning systems should also be integrated with existing patient management systems.
NICE recommends that all staff caring for patients in acute hospital settings should have competencies in monitoring, measurement, interpretation and prompt response to the acutely ill patient appropriate to the level of care they are providing.2 Ongoing education and training for all staff (including bank nurses) on use of early warning scoring systems will be key to successful implementation and to ensuring continuing competency.
The Royal College of Physicians, Royal College of Nursing, National Outreach Forum and NHS Training for Innovation have developed an online educational programme to train and support NHS staff in the use of the NEWS system. The e-learning tool is available at: http://tfinews.ocbmedia.com/
There is a lack of reliable evidence about whether to adopt and/or how best to implement electronic early systems. To support local decision-making, those already investing need to improve collection and reporting of how systems are being implemented, resourced and experienced in the NHS. To better inform the wider spread and adoption (or indeed discontinuation), there is a need to standardise both collection and reporting methods so that data are systematically captured in a generalisable format.
References
-
Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf. 2012; 21 (9): 709-712.
-
National Institute for Health and Care Excellence. Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital. (NICE CG50) London: NICE, July 2007.
-
Royal College of Physicians. National Early Warning Score (NEWS): Standardising the assessment of acute-illness severity in the NHS. Report of a working party. London: RCP, 2012.
-
NHS Services, Seven Days a Week Forum. Evidence base and clinical standards for the care and onward transfer of acute inpatients. December 2013. Available at http://www.england.nhs.uk/wp-content/uploads/2013/12/evidence-base.pdf
-
McGaughey J, Alderdice F, Fowler R, Kapila A, Mayhew A, Moutray M. Outreach and Early Warning Systems (EWS) for the prevention of Intensive Care admission and death of critically ill adult patients on general hospital wards. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD005529. DOI: 10.1002/14651858.CD005529.pub2.
-
McNeill G, Bryden D. Do either early warning systems or emergency response teams improve hospital patient survival? A systematic review. Resuscitation 2013; 84(12): 1652-1667.
-
Alam N, Hobbelink EL, van Tienhoven AJ, et al. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation 2014; 85(5): 587-594.
-
Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Archives of Internal Medicine 2010; 170(1): 18-26
-
Prytherch DR, Smith GB, Schmidt P, Featherstone PI, Stewart K, Knight D, Higgins B. Calculating early warning scores - a classroom comparison of pen and paper and hand-held computer methods. Resuscitation 2006; 70(2): 173-8.
-
Mohammed M, Hayton R, Clements G, Smith G, Prytherch D. Improving accuracy and efficiency of early warning scores in acute care. Br J Nurs 2009; 18(1): 18-24.
- Schmidt PE, Meredith P, Prytherch DR, Watson D, Watson V, Killen RM, Greengross P, Mohammed MA, Smith GB. Impact of introducing an electronic physiological surveillance system on hospital mortality. BMJ Qual Saf bmjqs-2014-003073 Published Online First: 23 September 2014