IHT Annual Meeting 2004
2nd Annual Meeting 3 November 2004
Hamilton House, London
"Delivering and Experiencing Innovative Health Technologies: Users' Perspectives"
This year's IHT meeting was attended by just over 100 delegates that included not only academic members from the Programme but also representatives drawn from community health, PCTs, patient groups, the media, health professions and policy makers. We were keen to explore the implications of IHTs for those delivering and using them so our focus was on how new technologies are made sense of and given utility in clinical and non-clinical settings. A drug regime, a genetic screen, a new test, but also popular technologies of information and communication, such as the internet, all figured in the debate. In some ways, our meeting was an exploration of the point made by US sociologist of science, Sheila Jasanoff (2004), who argues that 'the truths uncovered by science and the mobile objects that science authorizes must ultimately be received back into the humdrum rhythms of ordinary lives and localized experience in order to "work" right. When scientific knowledge or the technologies it sustains radically fail to fit their contexts of use, impossible confusion and loss of order can result.'

Andrew Webster
The Programme Director, Andrew Webster, opened the day with a short paper (here) that sketched out the main research questions that would be addressed and which he organised around the three themes of the meeting: managing chronic illness, risk calculation and technologies found 'beyond the clinic' among 'expert consumers'. He argued that 'the' patient is today a much more heterogeneous category - such as 'the expert', 'the intelligent', and the 'digital' patient - than is defined via the confines of the 'sick role' model. At the same time, it is crucial to locate the experience of IHTs within people's (not just patients') wider experience of health care, and how far this shapes or is disturbed by innovation in the clinic. The uncertainties as well as promise of drugs, devices, therapies and so on are mediated by our perception of health and its place and definition in our personal lives. As such, any new technology is embodied and expressed in ways that cannot be simply defined in terms of 'evidence-based' medicine or the metrics of clinical outcomes. These criteria are important, of course, but they are more about efficiency of resource use than about the actual experience of medicine, and they can not only be contested but are much less predictive of good health than might be presumed.
This was evident through the first principal speaker of the day Paul Flowers, whose team explored the impact of HAART (Highly Active Anti-Retroviral Therapy) on those who are HIV positive (see here). He not only showed how the medicalisation of HIV has turned the condition from being a terminal disease to a chronic manageable infection (and thereby brought relief for many) but has also, in the way this has been done, made it difficult to assimilate the drug regime into everyday life for those who find themselves locked into it - as one respondent said, like 'a marriage'. At the same time, the move towards a biomedical solution has created some loss, inasmuch as it has led to a narrowing of clinical care such that the focus is on drugs not the patient body or their experience of the illness. It was, he argued, crucial to re-engage with the psychosocial dimension of ill health if HIV treatment was to be more effective.
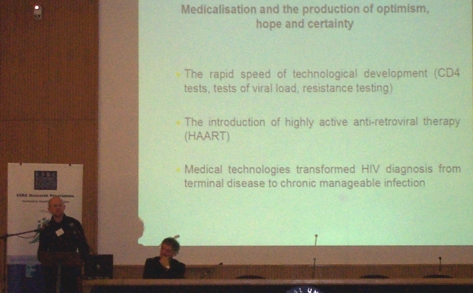
Paul Flowers
Frances Griffiths and her team described their work (here) on bone densiometry as part of a larger project exploring women's mid-life and the ways they respond to the increasingly medicalised disorders experienced then. Densiometry is used as a way of determining a woman's brittleness of bone or osteoporosis and so whether she should take some therapeutic measure such as HRT. Frances showed how the women in their study sought - though this was impossible - some certainty from the bone testing clinicians provide about their state of health. Such tests are only population based in terms of the measures they deploy and cannot predict the likely difficulties an individual herself will face. The team argue that clinicians need to avoid this and to acknowledge and help make sense of the uncertainties that characterise these tests and their meaning.
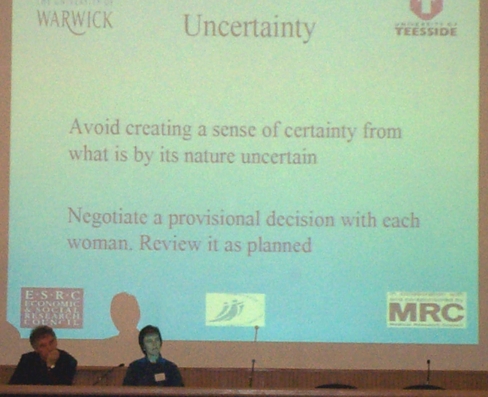
Frances Griffiths
Bill Noble, representing David Clark's research team explored the use of a range of pain relieving devices for cancer patients in palliative care. The project, recently completed, explores this as a clinical problem, a public health issue and a moral and ethical challenge. Over the past fifty years cancer patients have become more actively involved in their treatment and care, concepts of cancer pain have moved beyond the physical to encompass mental, spiritual and social suffering, and the understanding of pain mechanisms has deepened. The promotion of patient autonomy has been a driver of change - leading to the introduction of long-acting pain relieving drugs, special technologies for their delivery and the vision of individually tailored pain management. Bill showed that patient narratives about cancer and pain can be seen as evidence of the cancer patient's growing sense of self and self-worth that seeks to transcend and redefine patient hood; a growth which correlates with longer life expectancies, more treatment choices, growing societal activism and calls for autonomy. He reported that the growing patient voice is audible in cancer pain research, but not necessarily in the same language used in narratives written by patients themselves. This disconnection needs to be addressed through much closer liaison with patients.
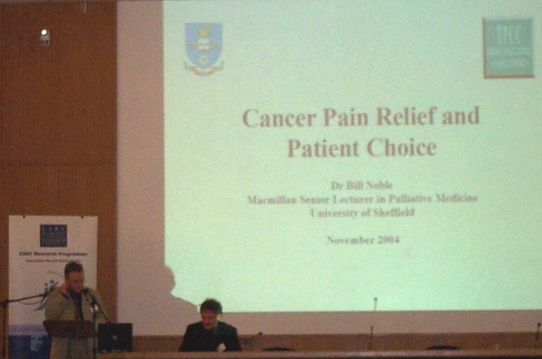
Bill Noble
Lynsey Beswick, our first guest speaker on the day, rounded off the morning with an eloquent and challenging presentation (here) about the disciplined, routinised and typically self-administered regime of health care that Cystic Fibrosis sufferers have to meet if they are to ward off distressing symptoms and live as everyday a life as they can. Lynsey herself has CF, works for the Trust, and described the existing IHTs that help cope with the disease, and the hopes for the future. But she also offered a powerful account of the difficulties these technologies pose, especially for teenagers, trying simply to be teenagers. Increasing longevity of sufferers meant that new social, cultural and personal questions and demands were raised that had no easy solutions, and certainly none that could be provided by 'the clinic' itself.

Lynsey Beswick
In the open discussion with all the presenters, a number of questions were raised by the delegates. One of these, that some of the papers had touched on, was the use of test results, on 'the numbers', to help diagnosis, yet they had criticised the ways in which these were often to lead to dubious senses of certainty. How could this be managed? One problem is that the technical limits of what is 'detectable' were constantly changing as technologies became more sophisticated. There is a need to keep certainty and uncertainty in balance, and a need for them to be defined beyond the parameters set by technical algorithms or standards themselves.

Some of the audience
Jane Sandall opened the afternoon session with her paper on the project her team has been undertaking over the past two years, examining the recent availability of first trimester (within the first 12 weeks or so) screening for Downs syndrome in antenatal clinics (see here). Typically most women are offered second trimester screening and the move towards a 'One Stop' earlier screen involves both a tightening and speeding up of the process. While the women for the most part valued faster results, early screening and having an early scan, Jane pointed out that the effect of this was to make what she called 'informed compliance' (rather than informed choice) more likely.
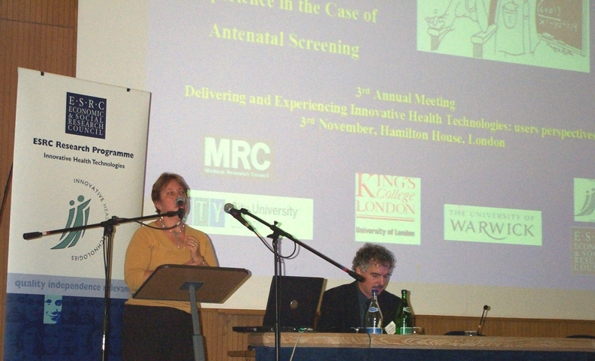
Jane Sandall
Jenny Hewison picked up (here) the reproductive technology theme with her team's presentation on prenatal screening and what women want from the advancing technologies in this area. Using a range of hypothetical scenarios of possible birth disorders her research finds that there is a major gap between testing and attitudes towards termination. Women wanted information about conditions for which they were not at risk, and the information was used primarily in the wider context of their family, personal situation and beliefs. There is a high degree of consensus amongst women from the different social and ethnic backgrounds included in the study about the conditions that justify termination of pregnancy. The conditions are few in number, and all have wide-ranging effects on the child, its parents and other family members. There was substantial individual variation in views about the other conditions, and the need for prenatal testing programmes to accommodate such variation was evident.

Jenny Hewison
Tom Quinn, professor of cardiac nursing, and the second guest speaker for the day, spoke about the risk of heart attack and risk management in acute conditions, typically during the first hour - the so-called 'golden hour' - when treatment should be started. This has led to the development of various early stage interventions by paramedics using decision support tools in the ambulance itself. Tom described how this has enabled much more effective early intervention, but has created its own professional side effects inasmuch as the locus of authority in managing the patient moves from the hospital doctor to the paramedic. This clearly raises governance and possibly legal issues too. His observations echo a number of findings from across the Programme - such as in NHSDirect - where it has been shown how IHTs disturb conventional professional and organisational modes of delivery.

Tom Quinn
Nick Fox opened the third session which was devoted to 'the expert consumer and user', and described (here) his Sheffield-based team's work on the use of the internet by consumers to secure drugs, for both lifestyle and health purposes. He spoke about the use of drugs to manage obesity and, in contrast, anorexia, and impotence, among different (lay) internet communities. In regard to the first of these, he explained participants' motivations to use the Internet to obtain pharmaceutical drugs. Engagement with the internet community supported participants' management of their weight condition and its treatment. In this sense, becoming an expert patient appeared as a radical, democratising process, giving the patient influence over treatment options. However, in using Xenical to 'treat' weight gain and 'normalise' the body, the users were - intentionally or unintentionally - accepting and perpetuating the medicalisation of body shape. In contrast, among anorexia discussion group, Nick's group found a different ethos. Like the previous community, it was an invaluable emotional and motivational support network, indeed, it established a subjectivity in its members in which anorexia was to be managed rather than cured. Within this 'anti-medical' and 'anti-recovery' ethos, weight loss pharmaceuticals were used to maintain low body weight, thus infusing these medicalised treatments with new meaning.

Nick Fox
A key issue discussed by Nick and in subsequent discussion was the question of governance and safety of free access to drugs on line. Nick felt that this opened up new opportunities for a consumer rather than solely producer/clinician based approach to the access and regulation of drugs. A range of consumers have established online communities, some of which are devoted to the use of pharmaceutical drugs for both intended and unintended purposes. There is a need to understand this diverse drug- consumer ecology and identify both the new risks and opportunities it may create.
Sarah Nettleton, from York, described (here) her team's work on e-health and the changing demography of the online population seeking health information, in a context where the very structuring of such information via the web (through search engines) is functioning not only in a technical sense but also in a political and social sense. Broadly, it works to confirm conventional forms of authority and advice, anchored in the traditional biomedical model. In this sense there is a congruence between the old and new media, and a renewal of established forms of knowledge. This, she argued, pointed towards a 'concordance' between the positioning of authorised knowledge on the web and its reproduction through the very search strategies and assumptions that information-seekers make in their own personal lives - a concordance between the 'macrostructual' and the 'ethnomethodological'. She examined six 'rhetorics of reliability' her team had identified in their fieldwork to demonstrate this process at work.

Sarah Nettleton
Tony Delamothe concluded, as our third guest speaker, with an interesting commentary on the internet version of the BMJ. As Web editor for the Journal, he commented on the use of information sources to provide, harvest and disseminate information in new ways. He noted how new technologies went through successive 'waves' and became increasingly integrated - where email, the mobile phone and web access might even act as a vehicle for telemedicine in extreme circumstances (one of which he described in graphic detail - frostbitten toes in Peru!). He spoke too about the 'Google-isation' of health information - among patients and doctors - and contrasted this to the more formal information systems - such as the NpfIT in the UK - being implemented today. The result was a diverse information space occupied by formal health providers, activists, patient and lifestyle groups.

Tony Delamothe
Finally, Nikki Ratcliff, of 'Which?' and a member of the Programme's Advisory Committee, rounded the day off with her comments on the event itself. She felt the meeting had helped delegates get a much clearer sense of the use of IHTs and the social and practical implications they have. Health is a consumer issue and healthcare has become something of a minefield for the patient, such that patient information is an essential part of a process that cannot simply be one-way: we need to ensure that health practitioners recognise that patient information needs can be highly individual and diverse, so what a 'patient's journey' is actually like will be a key question to ask, as will what degree of control over it that they have.

Nikki Ratcliff

Andrew Webster .......................Tom Quinn
.....Jenny Hewison .....Jane
Sandall
The meeting closed with news of forthcoming events and workshops, including a planned international symposium in Rome in June 2005, as well as the final conference that will be in October 2005. Details about this and other events will appear on the web site soon.
Professor Andrew Webster
Programme Director
November 16 2004.
