Ageing, Health Technologies and the Built Environment:
Developing a new research agenda
May 29 2003
Report on a joint ESRC, NHS Estates Workshop
1. Introduction
1.1 Three R&D programmes came together for the first time on May 29
- the NHS Estates research programme and two funded by the ESRC, the Innovative
Health Technologies and the Growing Older Programmes. The IHT Programme
initiated and organised the event. The aim was to pool expertise to answer
questions that each programme would find difficult to address individually.
We know relatively little about the link between the built environment and
the use of clinical technologies or how this relationship varies by age.
By exploring the ways these three dimensions come together in both clinical
and non-clinical (such as domestic) settings, this Workshop sought to identify
new ideas for intervention and therapy, and new areas that need to be researched.

Alan Walker
1.2 By linking these three research investments the following key policy questions can be answered:
- Can we improve our understanding of the relationship between ageing, health technology and the environment at either end of the life course where a high level of health and wider social resources (such as housing and social care) are deployed? Will this enable a more strategic and targeted use of such resources?
- How far can we derive lessons from research on the experience of ageing that can be transferred to the built and clinical environments?
- How far can we redefine health care as social care as we deploy new technologies in non-clinical settings, and so reshape the experience and meaning of support for older people? What are the practical and optimal limits to this?

Jonathan Milman
Presentation - ppt
2. What we found
The Workshop brought together academic, policy and user constituencies.
The Workshop papers, six in total, and the accompanying debate led to a
number of conclusions, as follows.
- Can we improve our understanding of the relationship between ageing, health technology and the environment at either end of the life course where a high level of health and wider social resources (such as housing and social care) are deployed? Will this enable a more strategic and targeted use of such resources?
There is a need to determine how personal biography and the ageing process from childhood onwards are linked to health and how a person's experience of health technologies their role and perceived utility change. Older people may seek a wider range of assistive technologies but feel more comfortable and compliant in their use if they fit in with what can be called their personal 'technographies', the broader engagement they have with a diversity of technologies, some directly related to health, others (such as IT) not. The more health technologies are designed for immediate use - especially diagnostic or monitoring devices in the home environment - the more we need to ensure these devices are not only effective but deemed to be useful and 'work'.

Morton Warner
Presentation - ppt
There is a desire to reduce the number of patients dealt with via hospitalised care - a supply-led approach premised on throughput of a large volume of (triaged) patients (and the inevitable creation of waiting lists where this fails). This also tends to produce hospitals that are very similar in terms of the design/clinical relationship. The research suggested it might be possible to move towards a multi-client, patient-centred design of both space and health delivery. Any move towards this undertaken in the context of the NHS modernisation programme and planned patient pathways might require a move towards a just-in-time health provision. Waiting lists for institutionalised care would decline rapidly were the locus and form of care to be redefined in this way. At the same time, however, patients suffering with co-pathologies make this more difficult to deliver.
Health demands are only partly predictable, and certainly unlikely to be stable over successive generations as social, demographic and economic developments reshape the pattern of health needs. The NHS needs to respond accordingly, and move towards more timely adaptation using just-in-time systems for acute care, while providing much greater support for carers for more everyday need. The recent move towards national training for carers is a step in the right direction.

Calbert Douglas
Presentation - pdf
Data analysis from one of the projects suggested that pilot substitution strategies that relocate geriatric care (for degenerative disorders) to the home might reduce current hospital bed needs - in the most optimistic case - by 85%. This is a huge reduction but would require a refocusing on local authorities (especially Housing Departments) and social services as key players in meeting health need.
There are important implications for the design of institutionalised care settings, where the move away from large volume throughput would suggest the adoption of a policy of specific designs for specific types of patient that need to be hospitalised. That is, we need to consider design from different patient groups. A major constraint on such a change is the current subscription to PFI, which tends to produce low-cost, standardised building. More generally, there are limitations to the degree to which it is possible to embed notions of home and homeliness into hospital settings, especially for acute care. Finally, national design protocols for diagnostic and treatment centres set by NHSE would need to be considered: they play a key role in regard to safety, public health and professional practice.

Thomas Scharf
Presentation - ppt
- How far can we derive lessons from research on the lifecourse that can be transferred to the built and clinical environments?
We know relatively little about how technologies and the built environment can be developed to support familial, residential and community 'normalities', especially people's engagement with the environment that is rooted in a sense of trust and security. But we have no clear guide as to what might be provided as a public good and what should be laid at the door of private choice: getting this wrong will simply reproduce existing forms of social exclusion, disadvantage and health inequality. These are already unevenly distributed in communities.
Complicating this issue, there seems at the same time to be evidence of a natural 'self-narrowing' on the needs for space and wider social engagement as people grow older. Can we try to determine whether this has implications for the public provision of services and health care?
More generally, the Workshop noted that we should attend to transitions across places of care, and seek to identify via longitudinal and intergenerational analysis how places of care can be designed to meet multiple or only more specific needs.

Sheila Peace
Presentation - ppt
- How far can we redefine health care as social care as we deploy new technologies in non-clinical settings, and so reshape the experience and meaning of support for older as well as younger people? What are the limits to this?
It is clear that there are major problems associated with the transforming of a specific space - such as turning a home into a space for clinical support. All space carries distinct resonances and meanings for those that occupy or use it, meanings that are not simply defined by the (health) needs of specific individuals but by the interaction of many others, such as siblings, the wider family, friends, visitors, professional practitioners and so on. The evidence from the papers also suggested that we might seek to press too far in de-institutionalising care by advocating home-based and self-care for the very old, some of whom may be suffering terminal illness: for many patients active support from trained practitioners was preferred limiting the burden on the immediate family.
The projects reported how technologies themselves are transformed as they are localised and customised in different settings by those that use them, such as assistive technologies in the home that sustain children who might otherwise be hospitalised. Technologies are not just 'taken up', since their users - whether patients or professionals (nurses, social services, clinicians etc) - must have both an absorptive capacity to use as well as an ability to make them workable, which might mean changing them, being selective in how or when they are used.

Jan Heaton
Presentation - ppt
3. Future Research Needs
In light of the above, the Workshop identified a number of areas for future research:
- How far does user-led (patient/resident-led) understanding of the delivery of service, and quality of environment shape effective intervention?
- How far does the context of use of health technologies determine their meaning, perceived value and health outcomes?
- How might these vary by technology sector, such as IT: do, for example, particular information interfaces make more or less sense across the life course as needs and interests change?
- How far are measures of 'quality of life' informed by patients, carers and residents in different neighbourhoods?
- How can new methodologies that are more participative be developed, especially for older populations not least to ensure stronger relations between designers of the environment and technology and their occupiers/users?
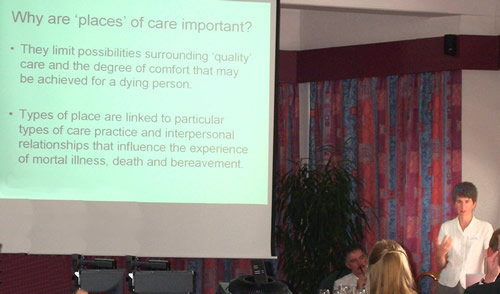
Jane Seymour
Presentation - ppt
4. Next steps
The Workshop co-ordinators will meet with interested parties to seek to develop pilot proposals that can address these issues. There would also be a need to bring local authorities and social services on board in any future initiatives.
In addition, a special issue of a leading international, but importantly interdisciplinary, journal will be published based on the workshop papers, and this will be edited by one of the project presenters.
Finally, the network of contacts from the meeting would be drawn on for future linked research in developing new research agendas targeted on different points in the life course.

The Panel
Judith Torrington Jonathan Milman Stuart Parker Alan Walker Andrew Webster
Further Reading
Lawson, B. (2002). "Healing architecture."
The Architectural Review. CCXI: 72-75.
Lawson, B. and J. Wells-Thorpe (2002). "The Effect of the Hospital
Environment on the Patient Experience and Health Outcomes."
The Journal of Healthcare Design and Development March: 27-32.
Lawson, B. R. and M. Phiri (2000). "Room for Improvement."
Health Service Journal 110(5688 20:1:2000): 24-27.
Lawson, B. R. and M. Phiri (2003). "The Architectural Healthcare
Environment and its Effects on Patient Health Outcomes."
London, The Stationery Office.
Useful Links
NHS National Knowledge Service Partners
http://www.nks.nhs.uk/partners.asp

